HIFU – Pioneering Advanced Ultrasound Technology for Prostate Cancer Treatment
by Dr. Amar Singh, MD Specializes in Urology
 Erlanger Hospital is proud to announce its position as the first healthcare facility in Tennessee to utilize advanced ultrasound technology to treat patients with prostate cancer. We now offer Robotic Focal HIFU (high-intensity focused ultrasound), a groundbreaking method for focal prostate treatment.
Erlanger Hospital is proud to announce its position as the first healthcare facility in Tennessee to utilize advanced ultrasound technology to treat patients with prostate cancer. We now offer Robotic Focal HIFU (high-intensity focused ultrasound), a groundbreaking method for focal prostate treatment.
Historically, the concept of a lumpectomy, as opposed to a radical mastectomy, for breast cancer was met with skepticism and resistance. However, it has since become the standard of care, significantly improving many women’s physical quality of life. Similarly, prostate cancer has been deemed unsuitable for focal therapy, or “lumpectomy,” due to the size and relative inaccessibility of the prostate, the multifocal nature of the disease, and concerns that focal therapy may limit treatment options in case of recurrence.
Today, thanks to Robotic Focal HIFU (high-intensity focused ultrasound), a prostate “lumpectomy” is indeed possible. Erlanger Health leads the way in Tennessee by offering HIFU, a specialized technology explicitly designed for focal treatment of the prostate.
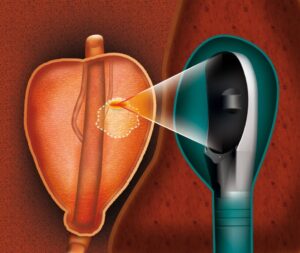
During HIFU treatment, targeted sound waves heat and burn the affected prostate area while preserving healthy tissue. This approach can potentially reduce the risk of side effects such as incontinence or impotence. HIFU has already been successfully used worldwide in Europe, treating over 65,000 patients. Encouraging results have been observed regarding both survival rates and quality of life.
A significant advancement in HIFU treatment is integrating ultrasound images with MRIs and biopsy data, known as “fusion HIFU.” By viewing the combined 3D images on a monitor, physicians can precisely focus the ultrasound waves, improving treatment planning and allowing for smaller margins around the cancerous tissue. This precision minimizes damage to healthy tissue, resulting in fewer side effects for prostate cancer patients undergoing HIFU procedures.
While HIFU may not be suitable for all patients diagnosed with localized prostate cancer, it provides a viable option for those who find active surveillance stressful or wish to avoid radical treatment such as surgery or radiation. HIFU serves as a middle ground between these two approaches, enabling patients to maintain their quality of life.
HIFU is a minimally invasive, radiation-free procedure that directs high-frequency sound waves through a probe inserted into the rectum. By selectively heating and destroying cancerous tissue while sparing healthy areas, HIFU holds promise in reducing the risk of impotence or incontinence. Internationally, HIFU has demonstrated positive outcomes, such as preserving continence for 97% of patients and erectile function for over 78% of men in a multicenter study conducted by the French Association of Urology (AFU).
The fusion of HIFU images with MRIs and biopsy data represents a significant leap forward in prostate cancer treatment. This fusion capability allows for enhanced targeting of diseased tissue during treatment planning, resulting in smaller margins around the contours of the tissue. By minimizing damage to healthy tissue, HIFU reduces side effects.
 Most women at some point get to have the experience of a urinary tract infection. This type of infection is commonly referred to as a UTI. According to statistics, approximately 10 million healthcare visits each year are attributed to this common problem. As much as UTIs may seem like just another annoying problem, there can be more to them than meets the eye.
Most women at some point get to have the experience of a urinary tract infection. This type of infection is commonly referred to as a UTI. According to statistics, approximately 10 million healthcare visits each year are attributed to this common problem. As much as UTIs may seem like just another annoying problem, there can be more to them than meets the eye. Every man has an innate knowing that his testicles are a delicate area of his body. Even the topic of
Every man has an innate knowing that his testicles are a delicate area of his body. Even the topic of
 Behavioral treatments for OAB include fluid reduction, diet changes, weight loss, and pelvic floor exercises. Bladder training (BT) is another means of behavior therapy for OAB that can be effective in a properly motivated or dedicated person. BT begins with education about overactive bladder often accomplished with brochures, websites or videos. Completing a record for several days of how often one voids (and whether there is an urgency to void) helps to identify a time interval of typical urination. The goal becomes to gradually increase that interval, usually by 30 minutes every 1-2 weeks. There are numerous distraction techniques (pelvic contractions, relaxation techniques) that can be used to ignore any urinary urgency that comes in between the interval.
Behavioral treatments for OAB include fluid reduction, diet changes, weight loss, and pelvic floor exercises. Bladder training (BT) is another means of behavior therapy for OAB that can be effective in a properly motivated or dedicated person. BT begins with education about overactive bladder often accomplished with brochures, websites or videos. Completing a record for several days of how often one voids (and whether there is an urgency to void) helps to identify a time interval of typical urination. The goal becomes to gradually increase that interval, usually by 30 minutes every 1-2 weeks. There are numerous distraction techniques (pelvic contractions, relaxation techniques) that can be used to ignore any urinary urgency that comes in between the interval. The authors detail the history of urethral dilation beginning in a time when very little was known about normal voiding. Dilation of the urethra emerged as a treatment for numerous problems including urinary tract infections and bladder pain. The assumption was that these issues resulted from a urine tube that was too narrow to permit proper emptying of the bladder. However, it is now known that spontaneous narrowing of the urethra (urethral stenosis) is uncommon and probably represents only 1-2% of patients with voiding dysfunction. This is much less common than the frequency of urethral dilation would suggest. One concern is that repeated urethral dilation can even be the cause of narrowing of the urethra due to fibrotic healing.
The authors detail the history of urethral dilation beginning in a time when very little was known about normal voiding. Dilation of the urethra emerged as a treatment for numerous problems including urinary tract infections and bladder pain. The assumption was that these issues resulted from a urine tube that was too narrow to permit proper emptying of the bladder. However, it is now known that spontaneous narrowing of the urethra (urethral stenosis) is uncommon and probably represents only 1-2% of patients with voiding dysfunction. This is much less common than the frequency of urethral dilation would suggest. One concern is that repeated urethral dilation can even be the cause of narrowing of the urethra due to fibrotic healing.
